By Dr Xavier Chee
The World Health Organization has designated antimicrobial resistance (AMR) commonly known as antibiotic resistance, as one of the most urgent public health threats in modern times.
In 2016, a team led by Lord Jim O’Neill published a scathing report emphasising the gravity of this situation. The report estimated that infections linked to antimicrobial resistance or AMR claim the lives of approximately 50,000 individuals in the US and Europe alone. Many more in other parts of the world are affected. If left unchecked, this figure could skyrocket to 10 million deaths by 2050.
An Accidental Discovery
In 1929, bacteriologist Alexander Fleming, a professor of bacteriology at St Mary’s Hospital in London, discovered the first antibiotic, Penicillin G, while conducting research on common staphylococcal bacteria. Fleming observed a petri dish near an open window that had become contaminated with mold, resulting in an absence of bacterial growth – a phenomenon that intrigued him. Conducting subsequent experiments, he concluded that a specific ‘mold juice’ was responsible for inhibiting bacterial growth.
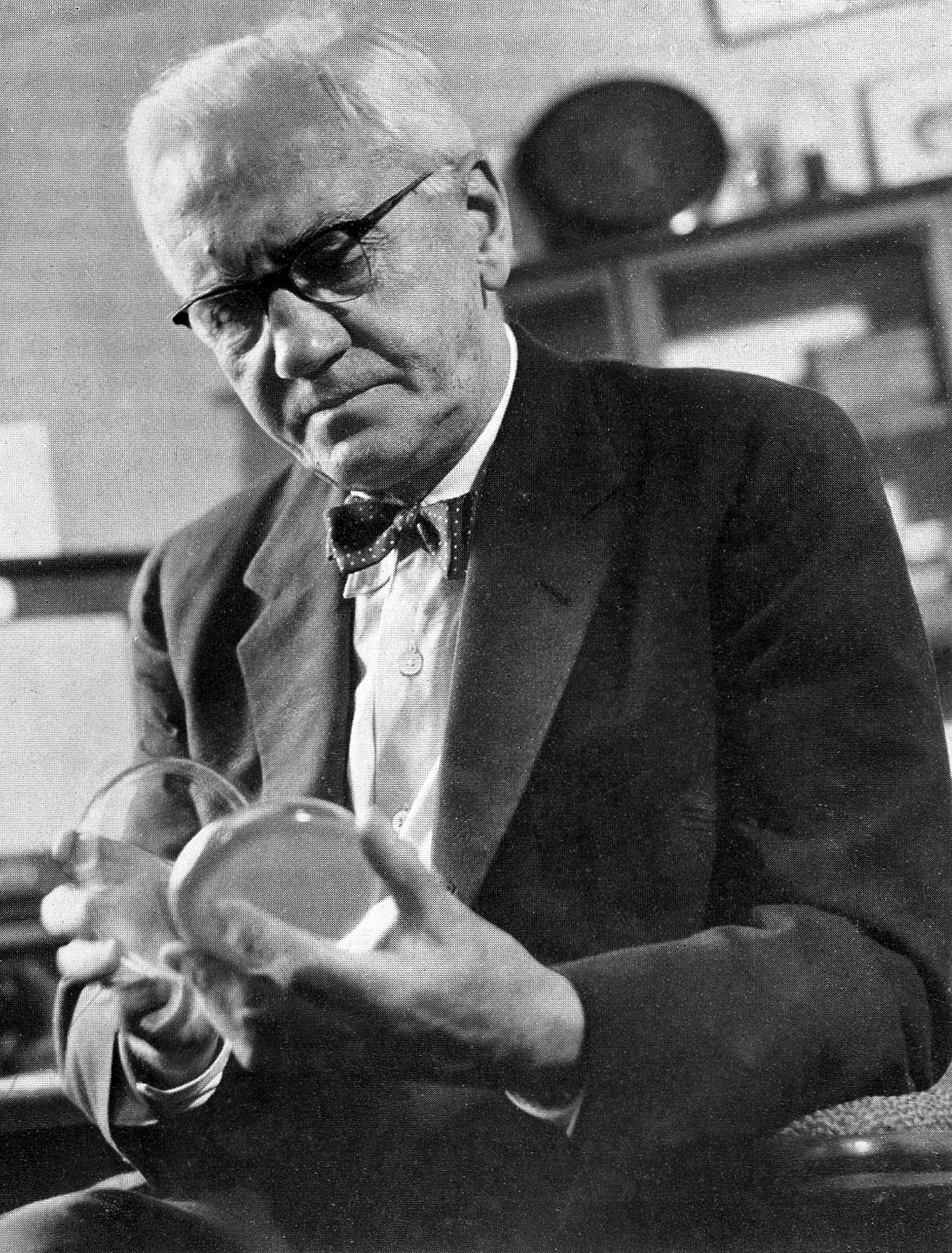
Sir Alexander Fleming. Wellcome Collection. Images@wellcome.ac.uk (http://wellcomeimages.org)
However, it wasn’t until 1940 that a team from Oxford University, including Ernst Chain and Howard Florey, successfully purified enough penicillin to treat a seriously infected police officer. Remarkably, the officer’s health improved within 24 hours of treatment with penicillin, only to tragically succumb when the supply of penicillin depleted.
At the time. the potential of penicillin seemed evident. However, during his 1945 Nobel Prize lecture, Fleming cautioned that “… not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body. The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant.” Decades later, his prediction of the ‘era of abuse’ came true.
The Misuse and Overuse of Antibiotics
Antimicrobial resistance can naturally occur without human intervention. It happens when bacteria adapt to and resist antibiotics, resulting in the antibiotics’ loss of efficacy, Nevertheless, the acceleration of AMR development has been propelled by humans through the misuse and overuse of antibiotics, insufficient implementation of infection control measures, inadequate hygiene practices, and the indiscriminate application of antibiotics in agriculture.
AMR jeopardizes every facet of healthcare especially the foundation of modern medicine. For instance, the National Health and Morbidity Survey 2019 indicates that about 3.9 million Malaysians suffer from diabetes. Diabetic patients face an increased risk of bacterial infections, which can spread rapidly due to elevated sugar levels. This scenario highlights how AMR could swiftly impact healthcare in Malaysia. More importantly, AMR’s impact extends beyond those afflicted with bacterial infections. Its progression could render crucial medical procedures like organ transplants, chemotherapy, and surgeries impossible. These patients, often with compromised immune systems, depend on antibiotics to prevent potential bacterial infections. The absence of effective antibiotics could transform routine surgeries into life-threatening situations.
A Global Economic Predicament
Beyond healthcare, the global economy would also suffer due to AMR. O’Neill’s report projects that over the next 35 years, around 300 million premature deaths could occur. The global Gross Domestic Product might decrease by 2 to 3.5% lower by 2050. This will contribute to a staggering loss of productivity worth USD60 to USD100 trillion due to AMR.
As voiced by Professor Dame Sally Davies, the Chief Medical Officer of England, “If we don’t take action now, we really are facing a dreadful post-antibiotic apocalypse.” The most troubling aspect of AMR is its silent progression leading to an impending crisis. Although the year is now 2023, there is still time for us to act. Addressing AMR requires significant efforts from every nation, strong political resolve, and substantial funding. However, in the words of Jim O’Neill, “The price of action is tiny in comparison to the cost of inaction.“
At this pivotal juncture, we simply do not have any other choice.
Dr Xavier Chee is a senior lecturer with the Faculty of Engineering, Computing and Science. His research interests include computational drug discovery methods, molecular dynamics simulation and machine learning in the treatment of diseases. Dr Chee is contactable at xchee@swinburned.edu.my

